Research Background
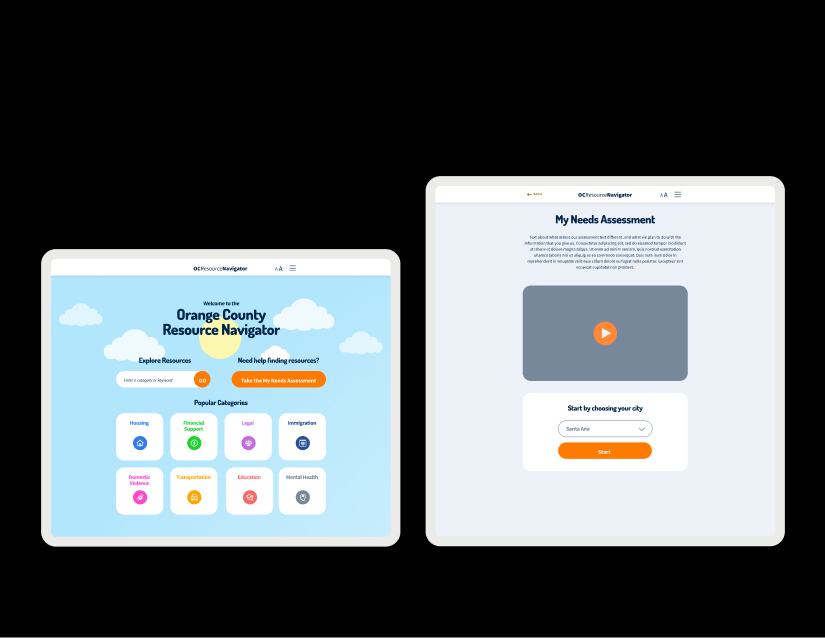
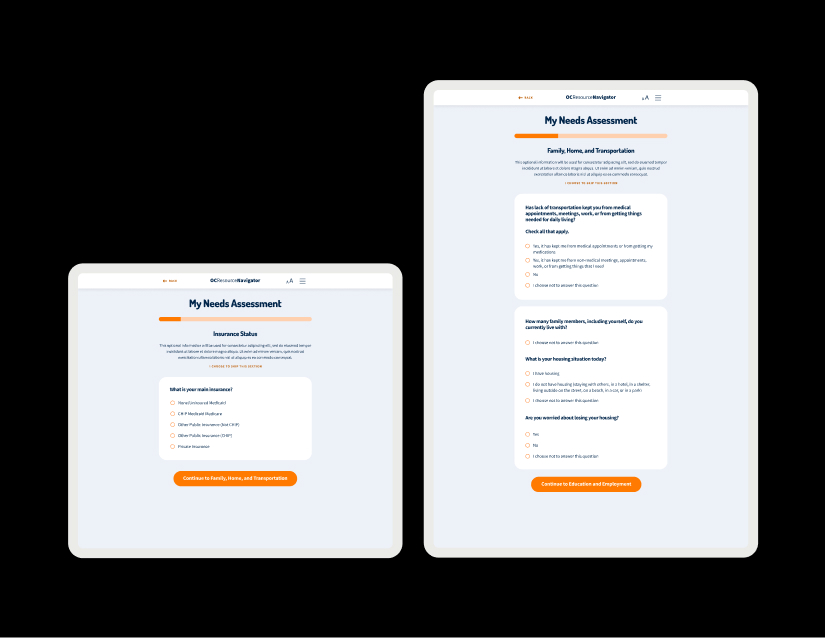
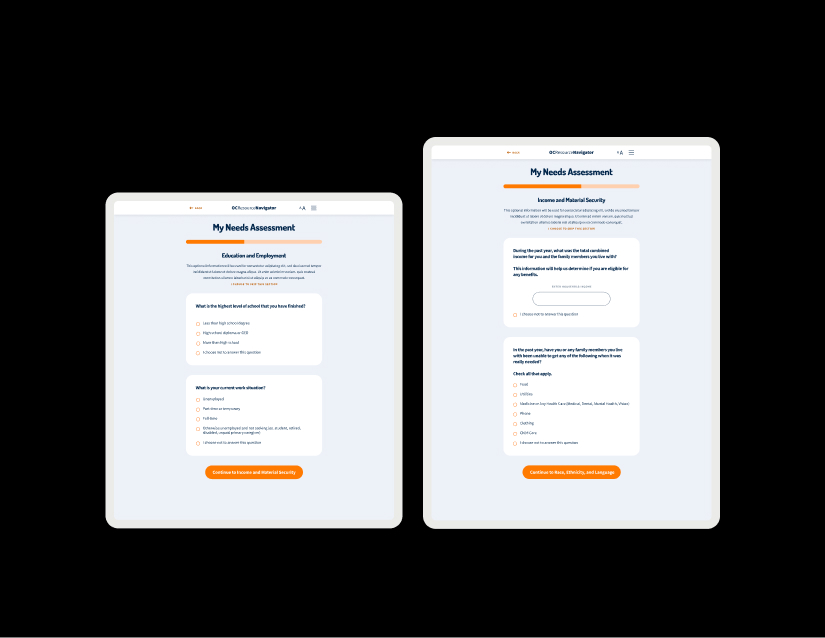
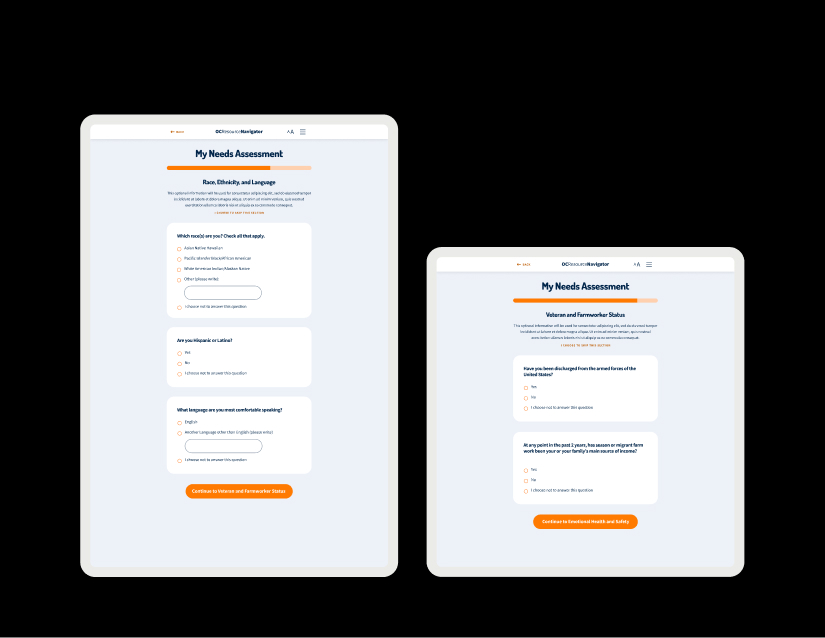
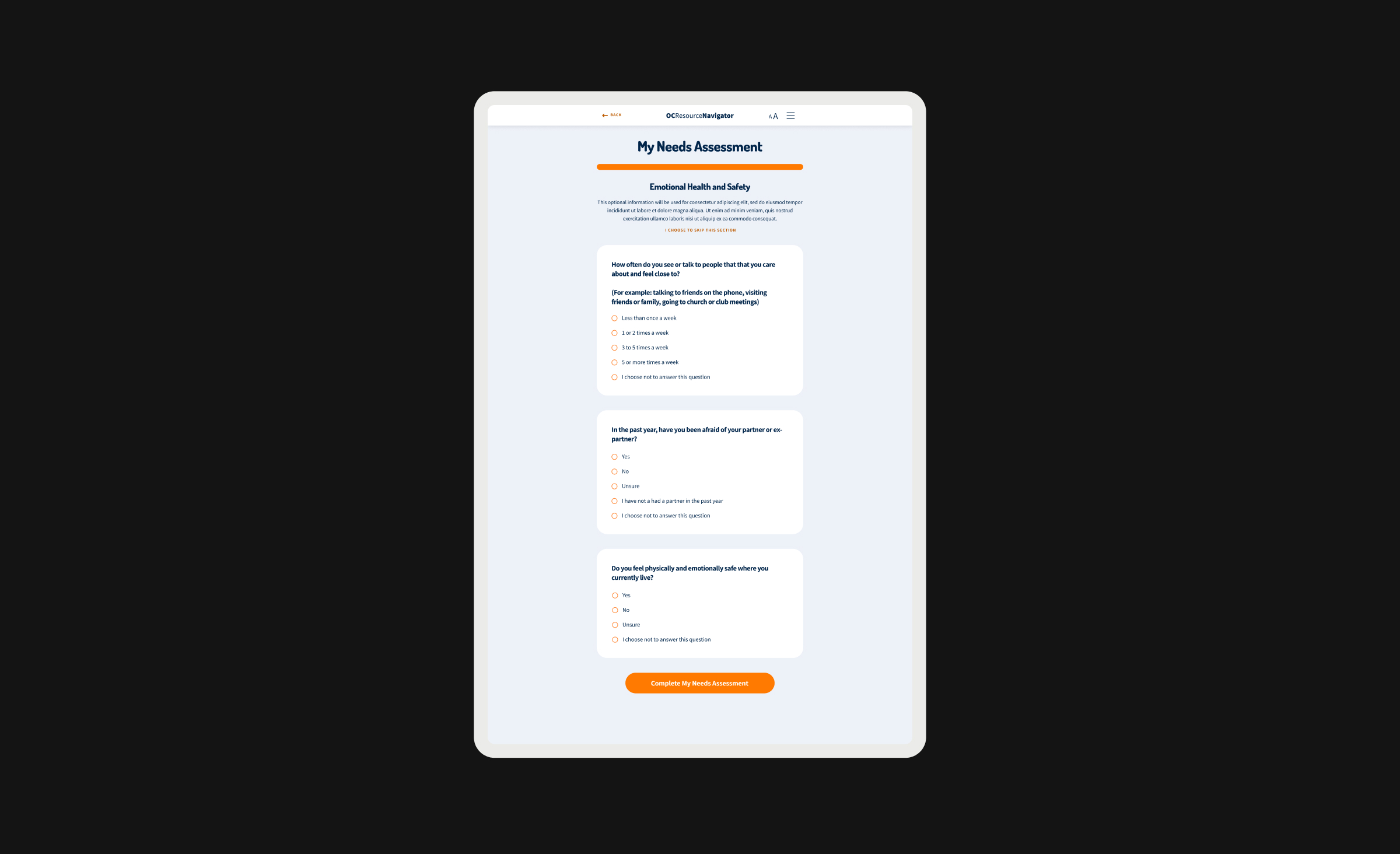
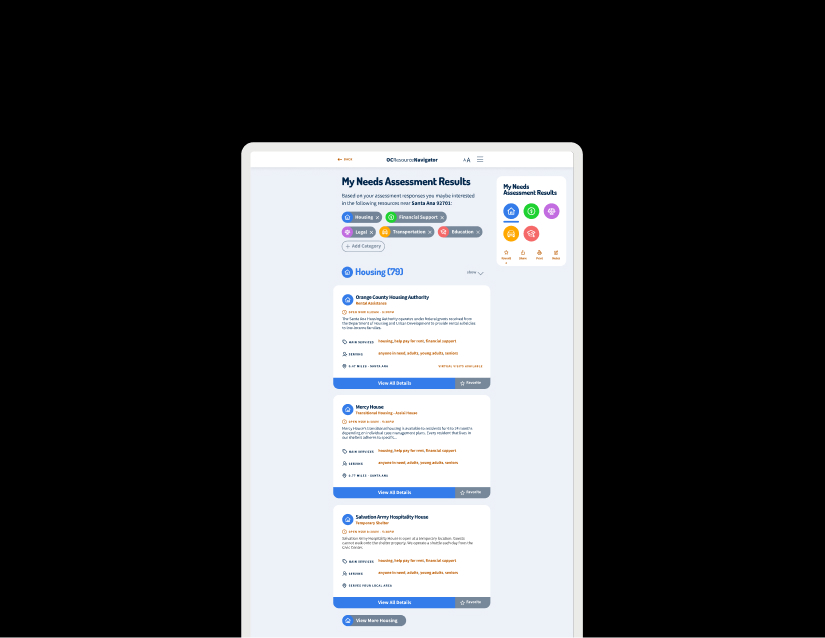
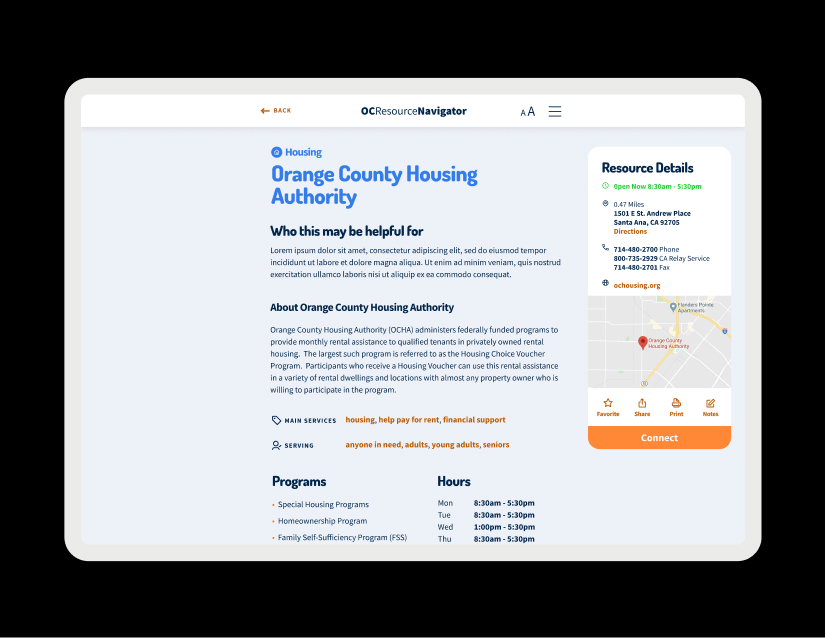
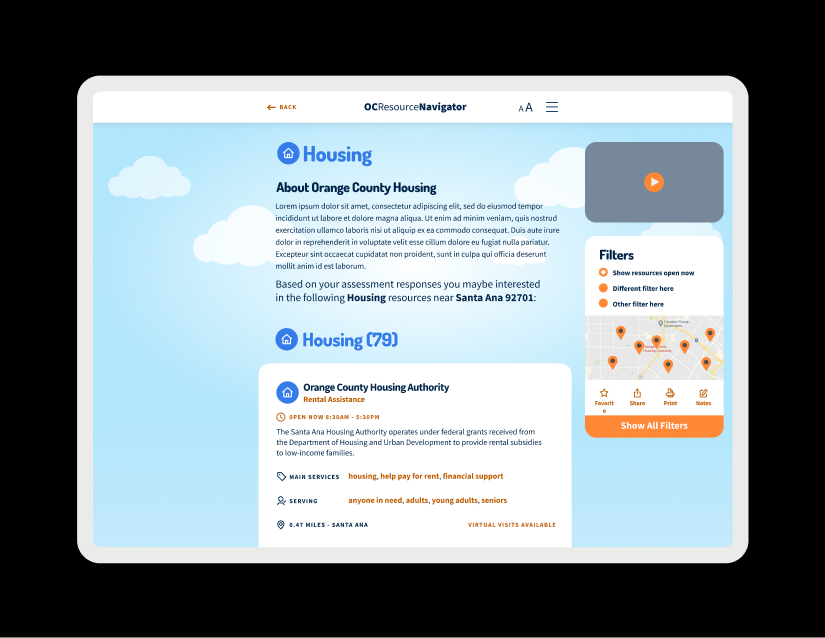
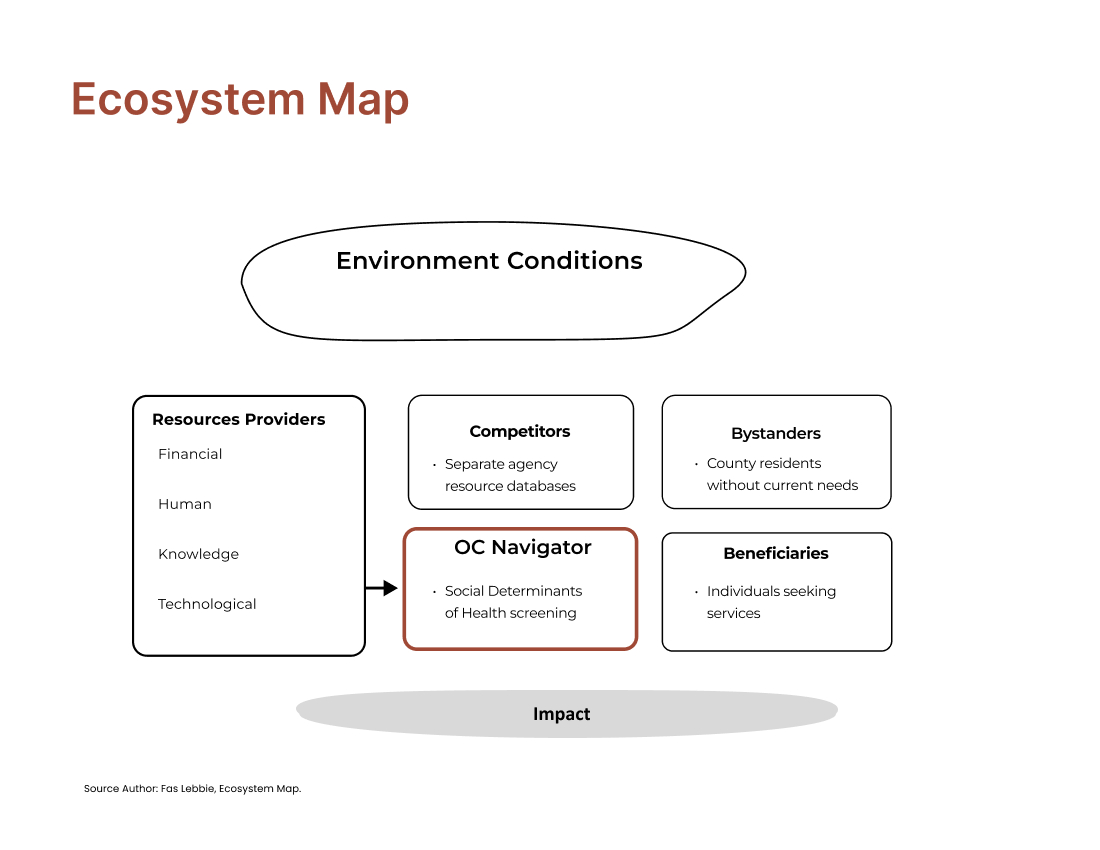
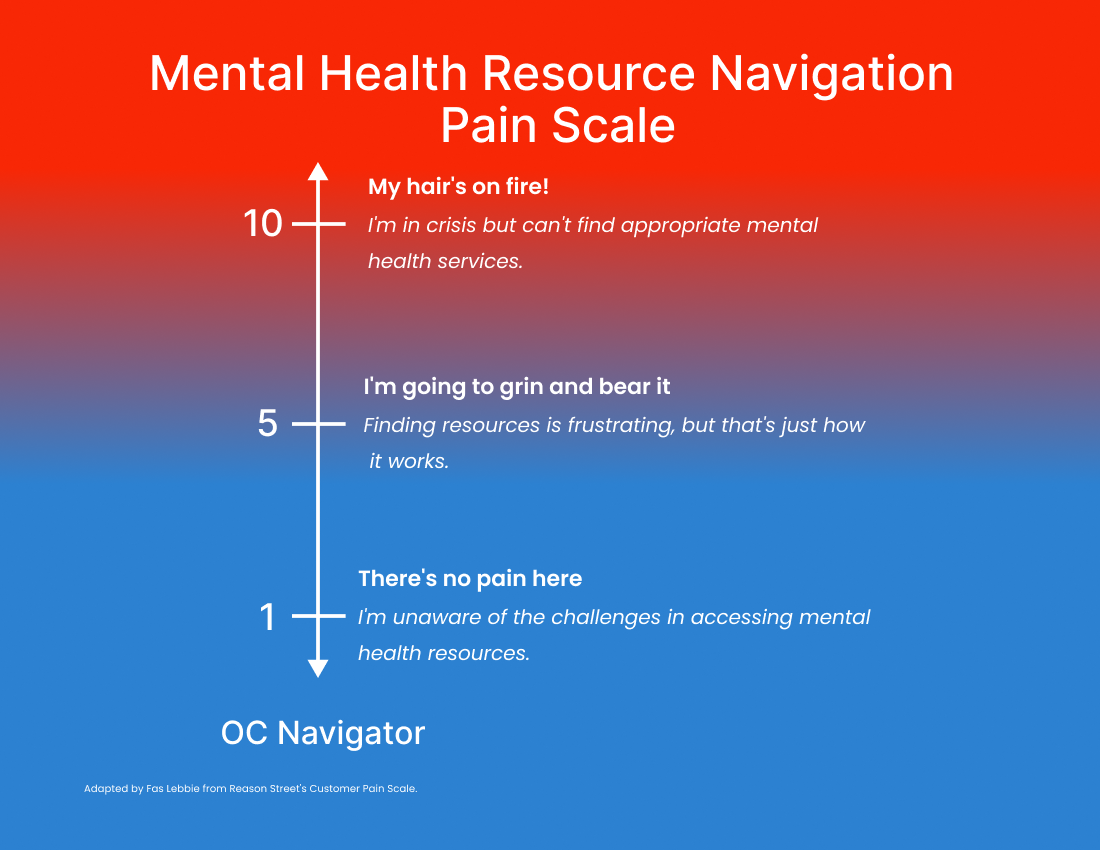
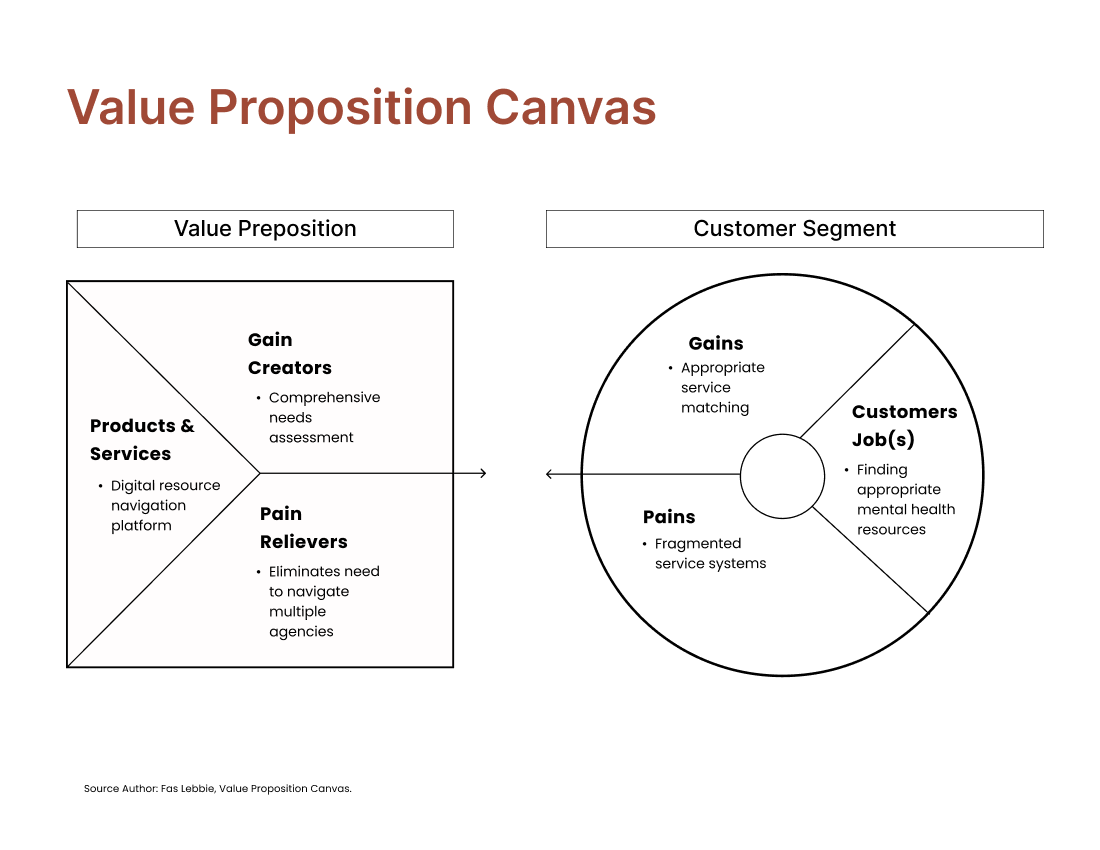
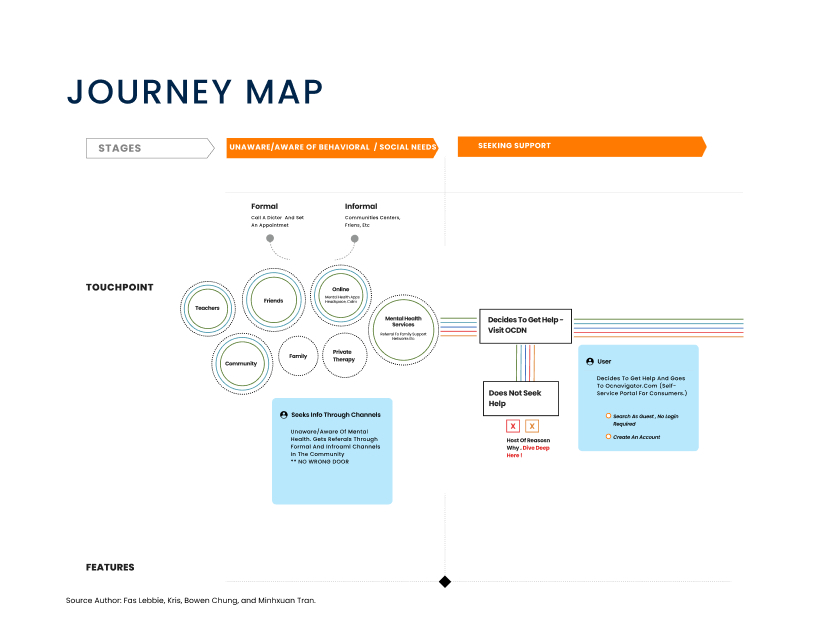
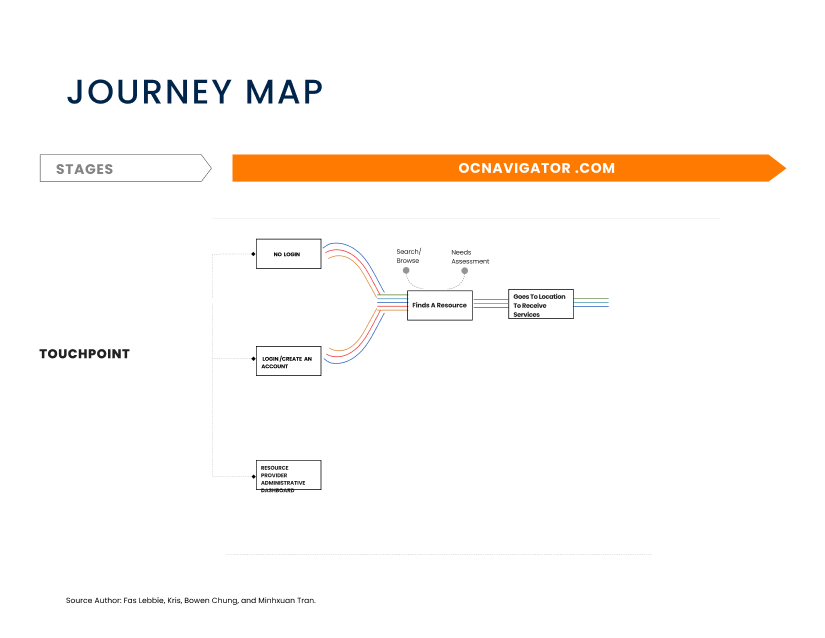
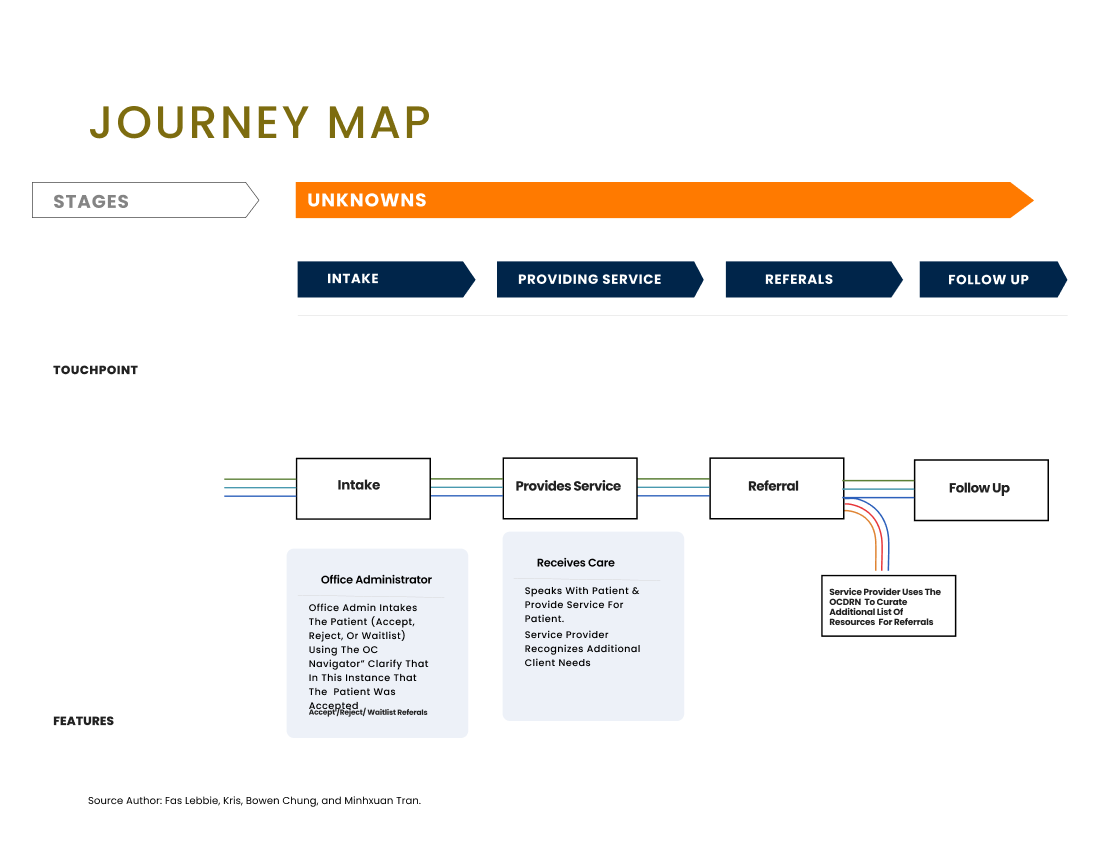
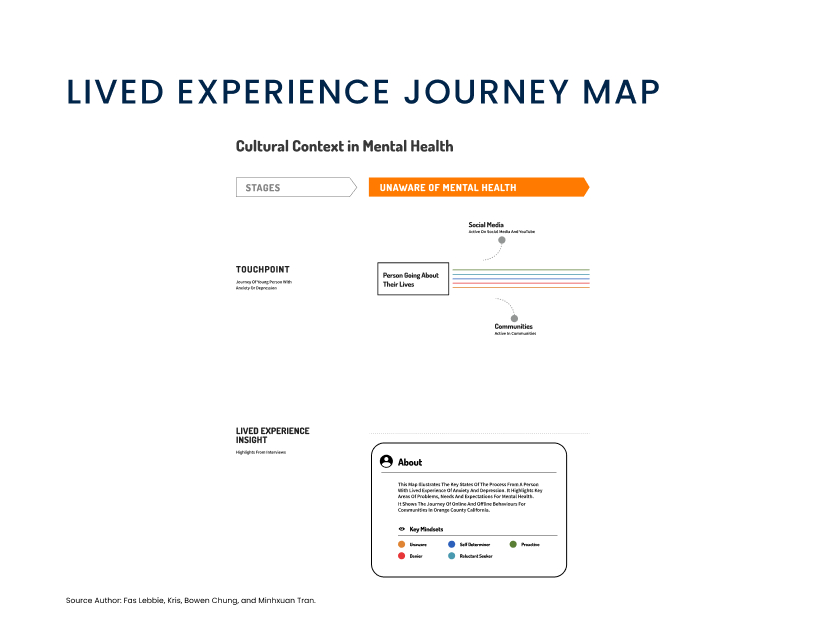
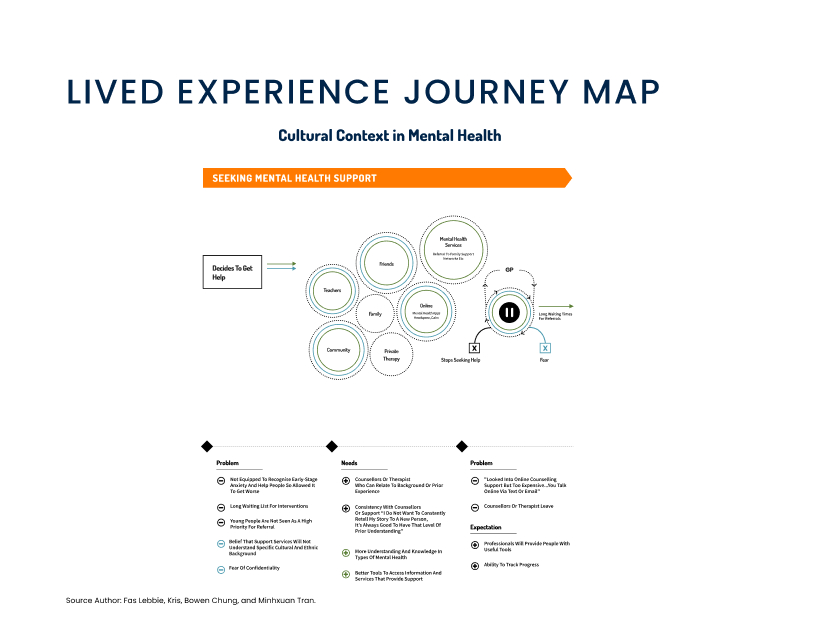
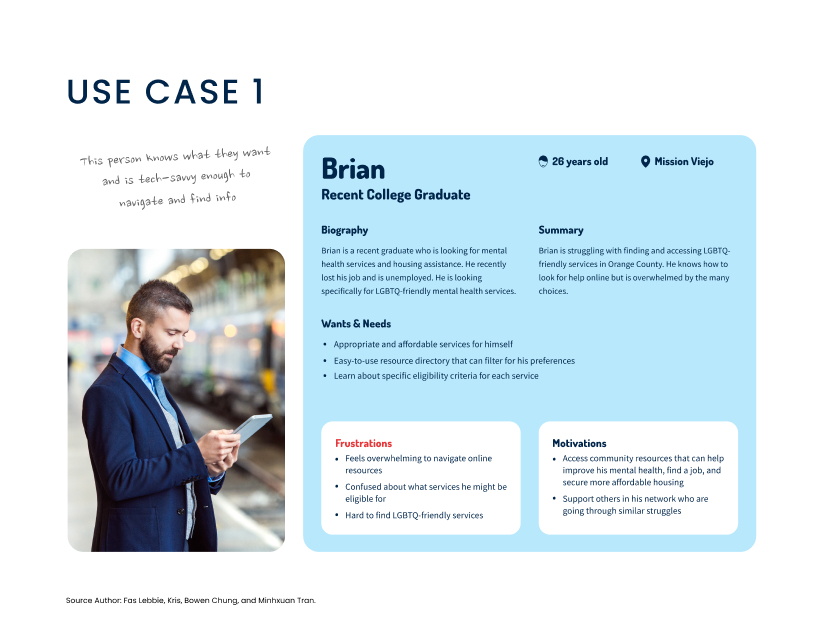
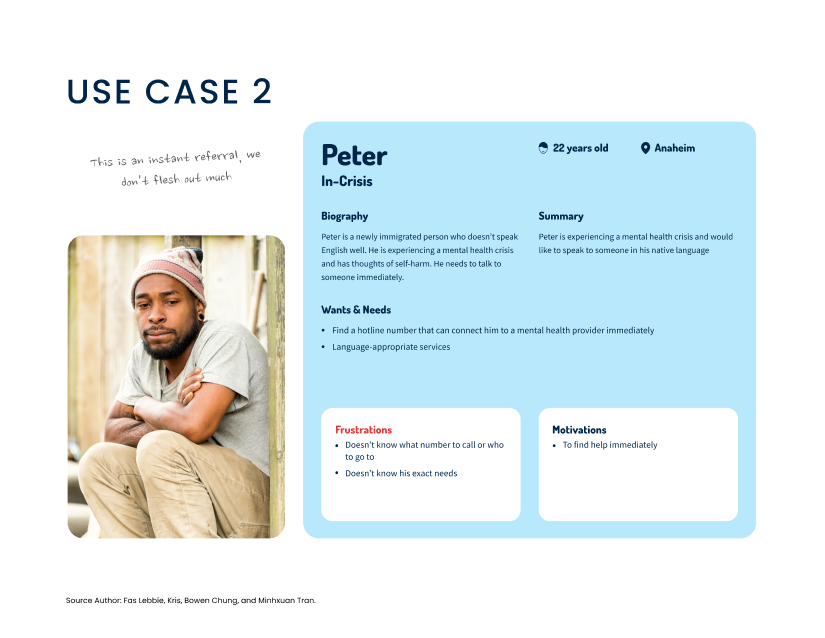
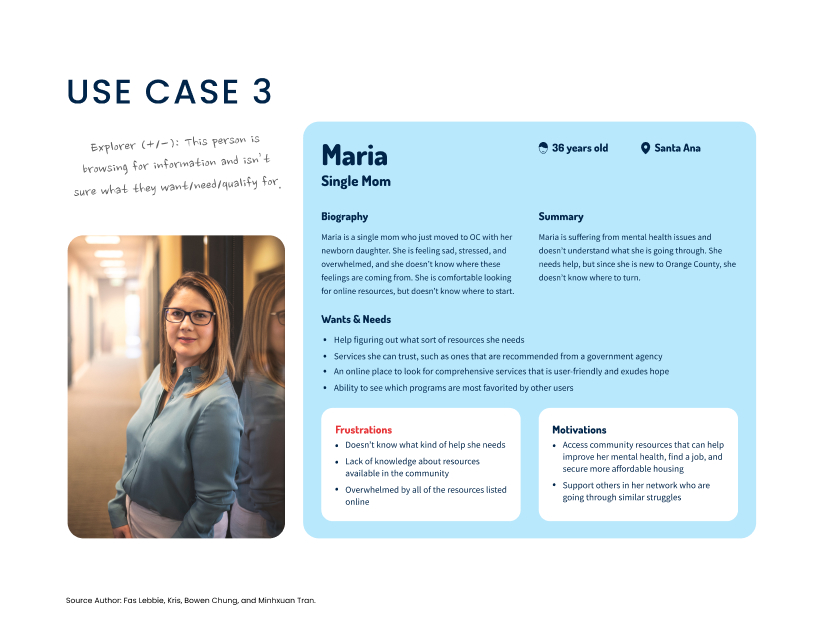
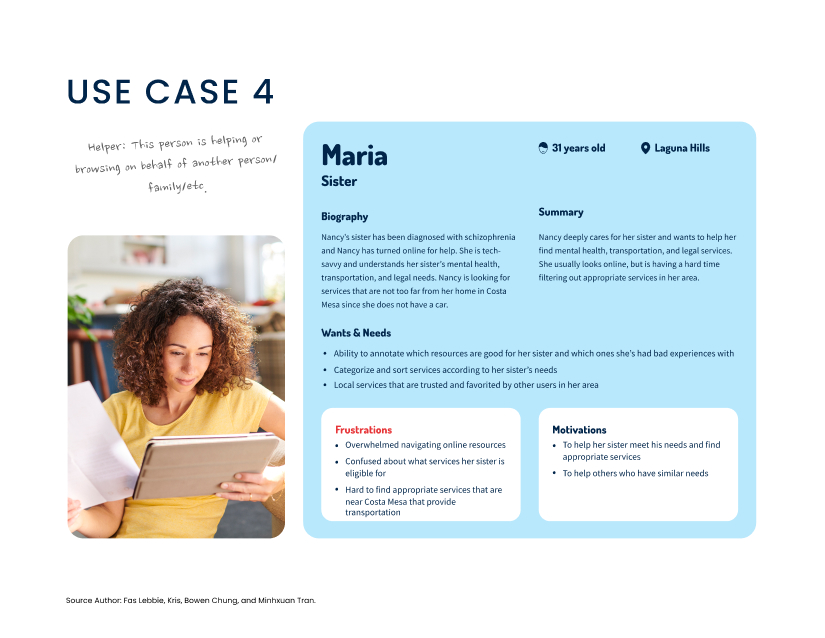
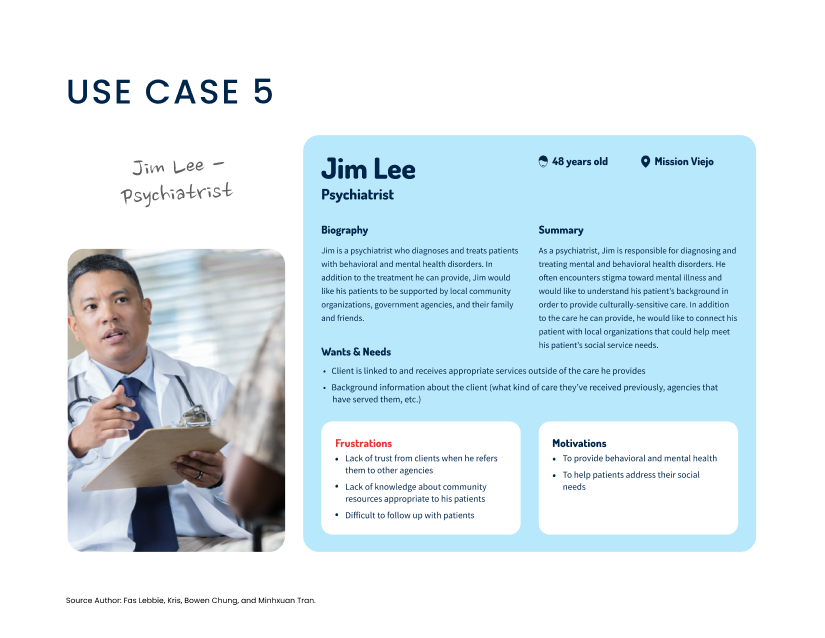
In Orange County, 20.7% of adults need help with mental health or substance abuse issues, but only 59% receive the care they need. This highlights a significant gap in mental health resource access, especially for diverse communities. COVID-19 has worsened these challenges, increasing anxiety, isolation, and social issues like housing and food insecurity. Resource hubs have gone virtual, intensifying barriers such as transportation, linguistic and cultural obstacles, and mental health stigma. The fragmented resource navigation system requires navigating multiple agencies, repeating stories, and meeting complex eligibility requirements. Public and private behavioral health systems lack coordination, and insurance networks often fail to support person-centered access and service delivery. Current care models focus on quantity-based measures over recovery-oriented outcomes, creating a disconnect between services and user needs. This fragmentation mainly affects vulnerable populations with limited English proficiency, technology access, or health literacy. Service providers maintain separate, often incompatible resource databases, causing confusion and missed care opportunities. By understanding the journey from recognizing a need to connecting with resources, there is an opportunity to create a more inclusive, responsive system that reduces barriers and enhances access to mental health support. The Navigator addresses this challenge by focusing on individual journeys rather than isolated system touchpoints. In Orange County, 20.7% of adults say they need help with mental health or substance abuse issues, but only 59% are getting the care they need. This shows there’s a significant gap in access to mental health resources, especially for diverse communities. Higher public and private behavioral health systems lack coordination, and insurance networks often fail to support person-centered access and service delivery. Current care models emphasize quantity-based measures rather than recovery-oriented outcomes, creating a disconnect between services and user needs.